The Diabetes and Metabolism Program includes both basic and clinical investigation into the mechanisms that lead to the development of insulin resistance and type 2 diabetes and seeks to identify novel approaches for the management, prevention and treatment of this disease.
Diabetes and Metabolism Program Research Areas
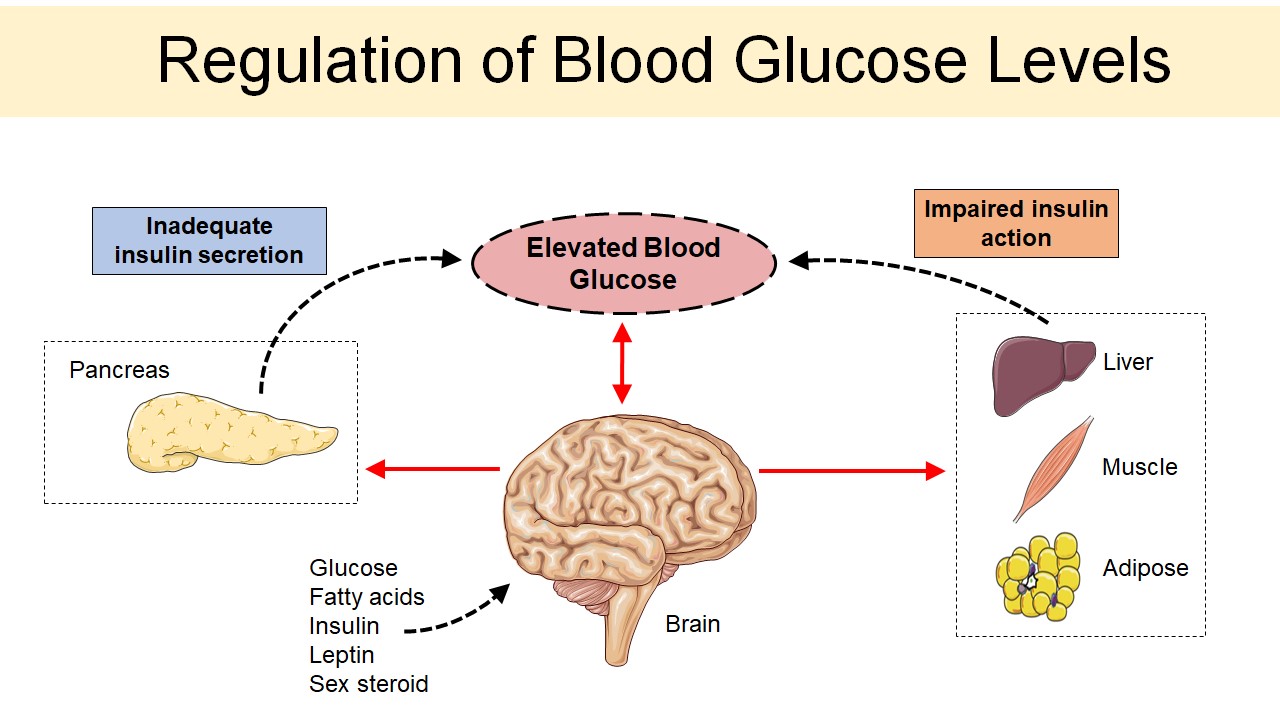
Diabetes is a disease that is characterized by persistently high blood glucose levels which, over time, may lead to nerve damage, heart disease, blindness, and kidney damage. Since the discovery of the pancreatic hormone insulin, most research has focused on the function of pancreatic islets in glucose homeostasis, advancing the idea that diabetes results from defects of insulin secretion, insulin action in peripheral tissues, or both. Despite these intensive research efforts, the incidence and prevalence of diabetes is increasing and current treatment options are limited. However, growing evidence indicates that the brain also plays a critical role in glycemic control and cooperates with the islet to maintain stable blood glucose levels. Thus, a better understanding of diabetes pathogenesis, including recognizing the important role of the central nervous system and crosstalk between different organ systems, is required to develop new strategies for the safe and effective treatment of this disease.
Our Diabetes and Metabolism Program covers both basic and clinical investigation into the pathogenesis of insulin resistance, inflammation, and central nervous system control of metabolism. Through strong collaborations and interactions between the diverse members of our research team, we are working to develop novel therapeutics for the prevention and treatment of type 2 diabetes.
Diabetes, Obesity and the Brain
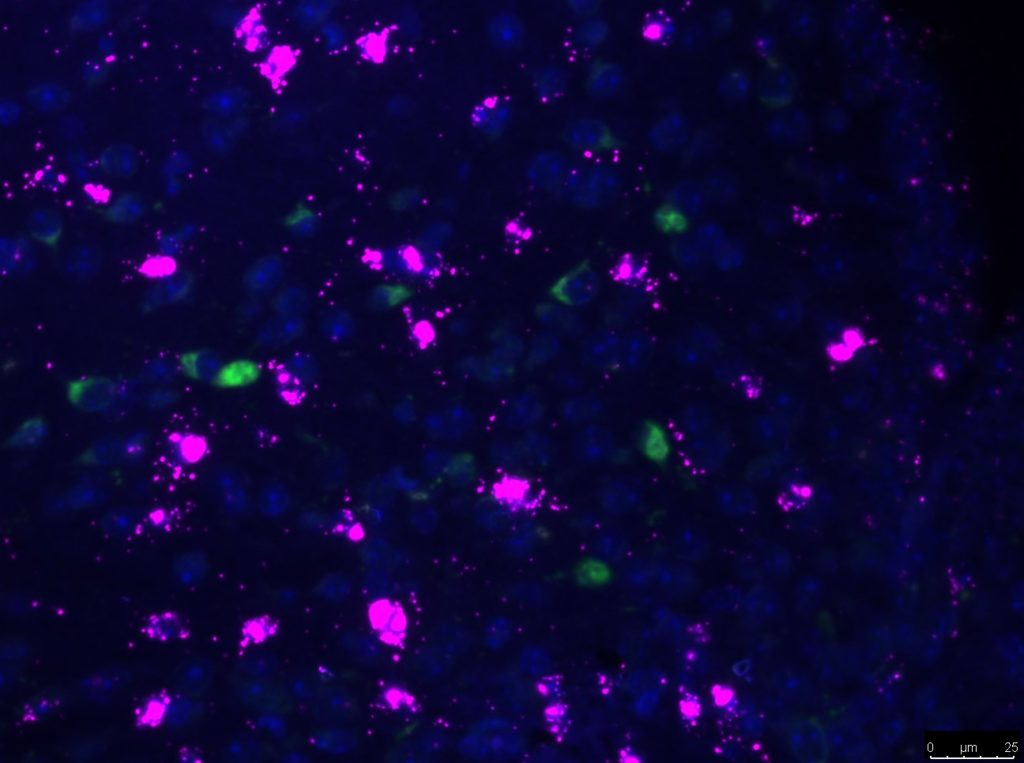
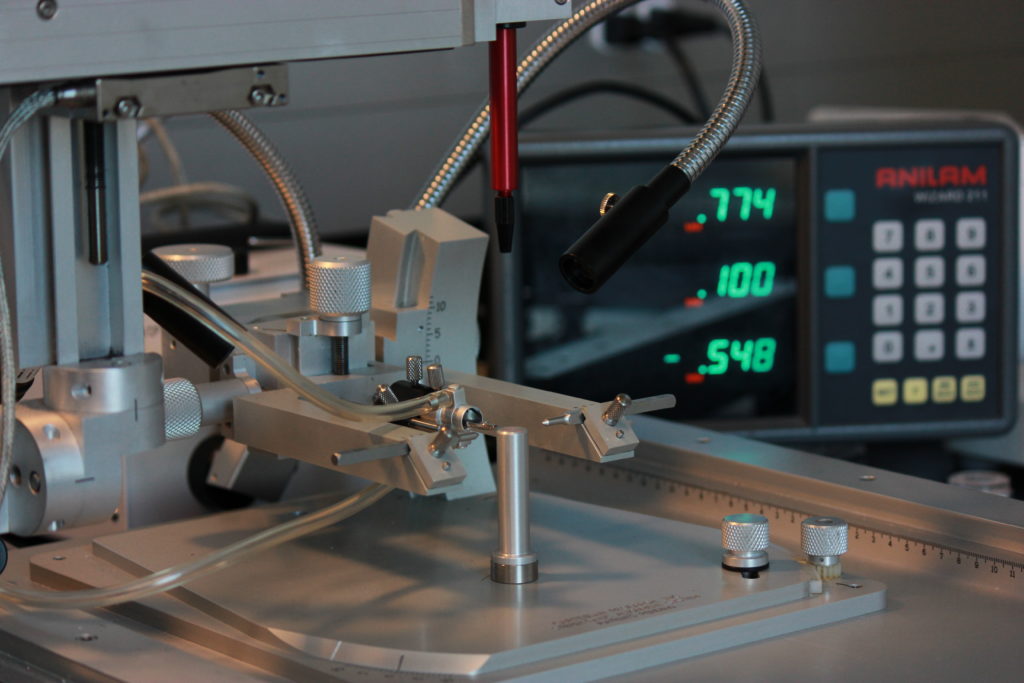
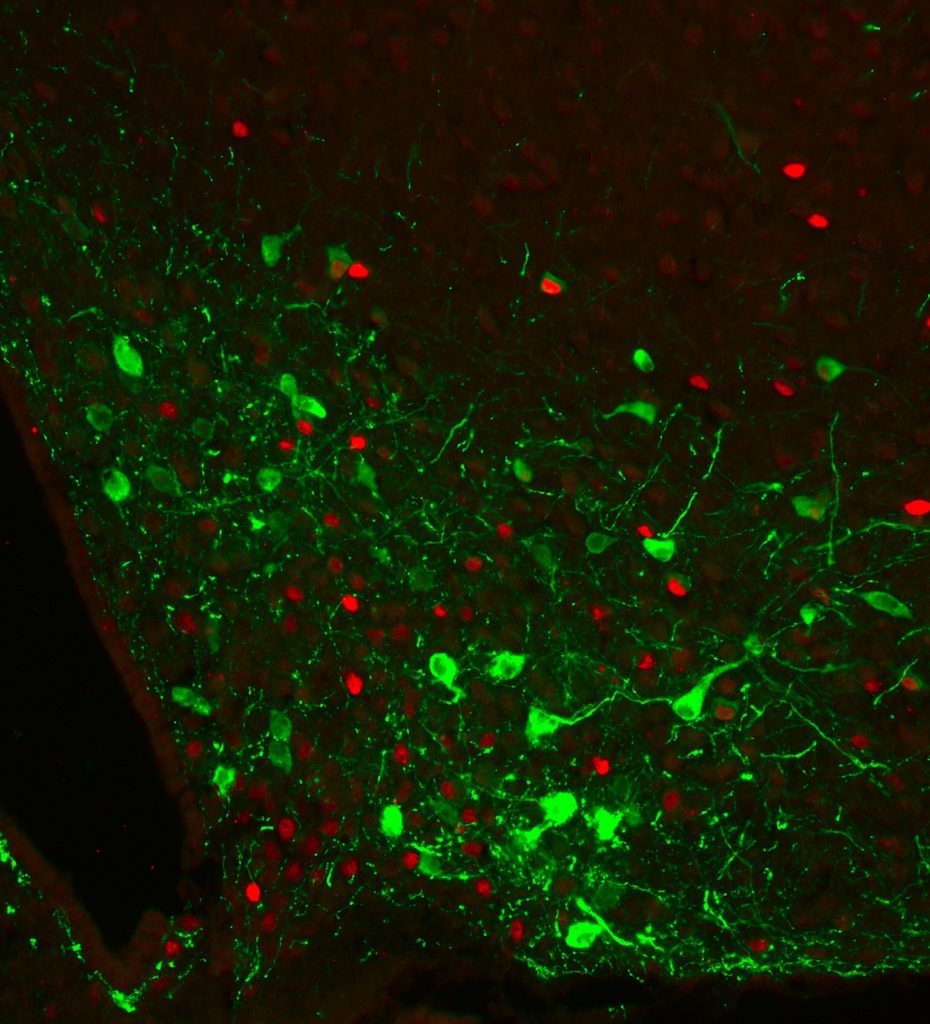
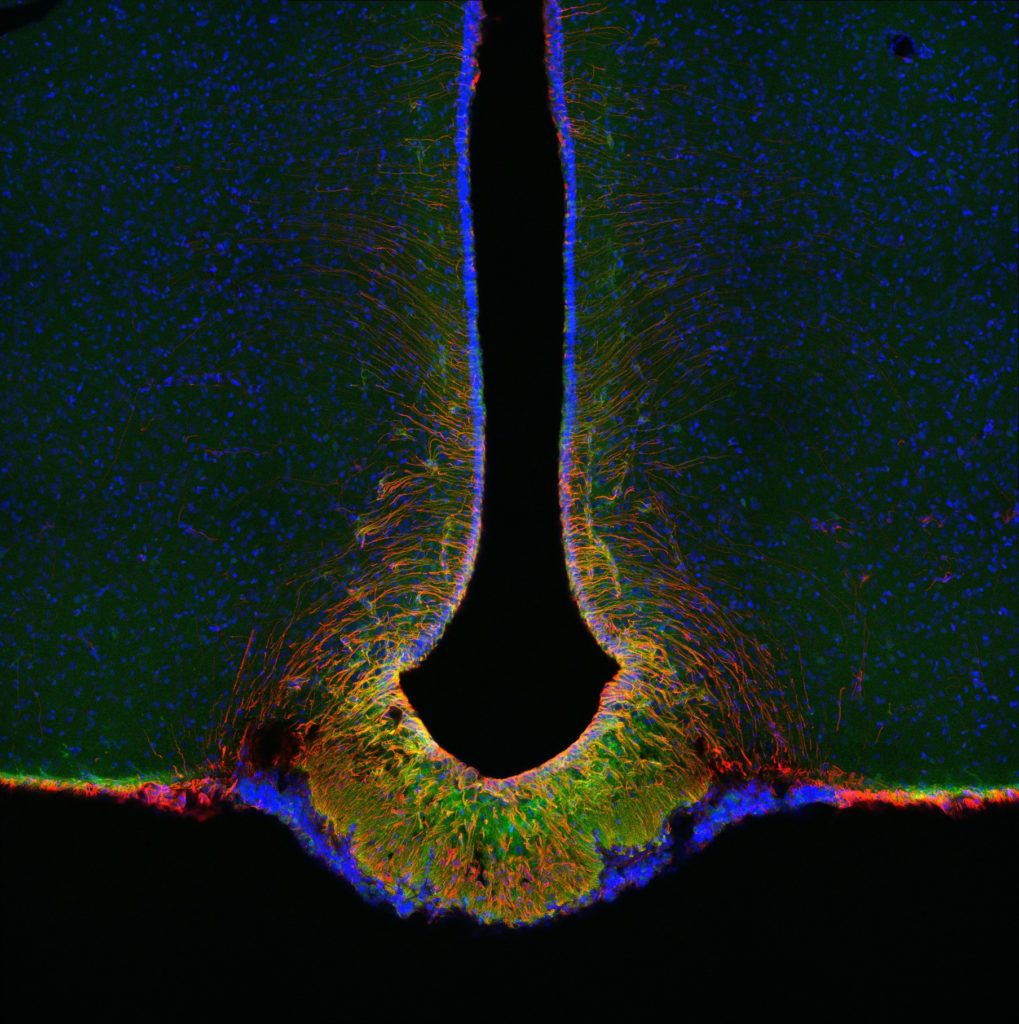
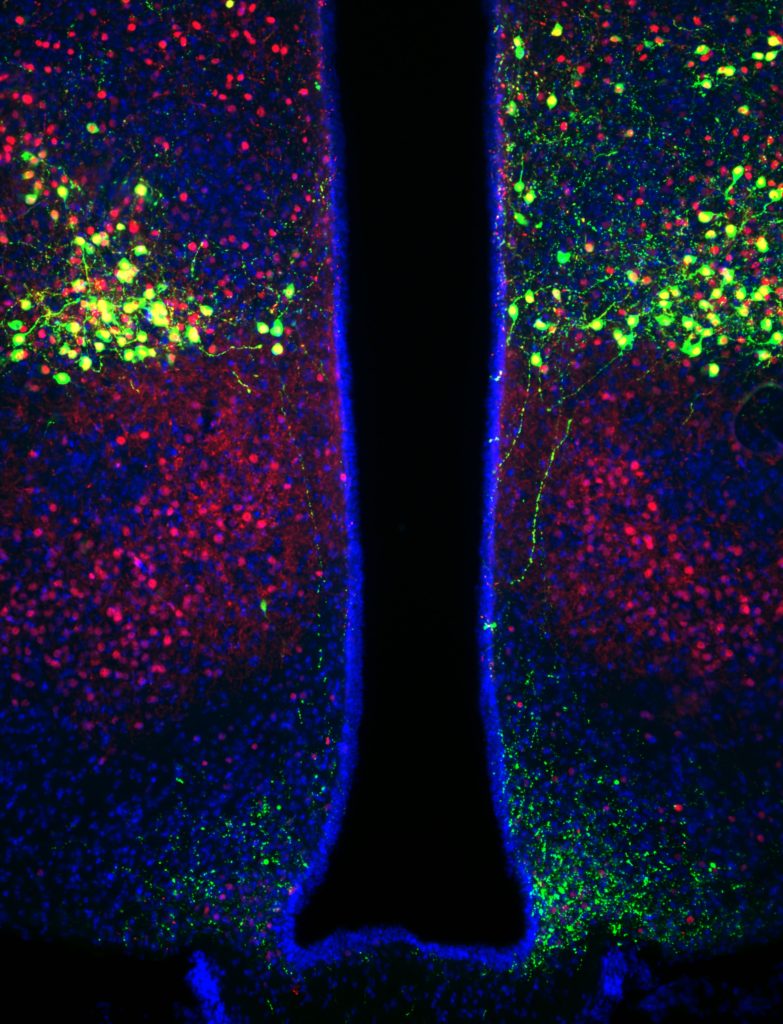
Members of this program study how the brain senses and responds to circulating hormones and nutrients from the periphery to maintain energy balance and blood glucose levels. Our work has shown that defects in this system contributes to the development of type 2 diabetes and obesity. Researchers utilize state-of-the-art neuroscience technologies including single-cell transcriptomics and optogenetics to identify and characterize novel cell types and brain circuits that regulate blood glucose levels. This research recognizes the brain as a novel therapeutic target with untapped potential for the treatment of type 2 diabetes.
Glucose Homeostasis and Diabetes Pathogenesis
Our research examines the actions of hormones and nutrients in peripheral tissues that regulate metabolism and control blood glucose levels. In addition to insulin-sensitive tissues such as liver and skeletal muscle, a particular area of interest is the role of adipose tissue inflammation to obesity-related insulin resistance and type 2 diabetes.
Nutrition, Hormones and Diabetes
Researchers in this program use basic and clinical studies to examine how diet, exercise, or pharmaceutical and surgical interventions can be used to treat and prevent type 2 diabetes. Research interests include how sex hormones affect insulin sensitivity, the effects of dietary and pharmaceutical treatments on energy and glucose homeostasis, and the mechanisms underlying the metabolic benefits following bariatric surgery.
Diabetes, Obesity and the Brain
William Banks, MD
View Department Profile
We investigate changes in the brain vasculature and blood-brain barrier that relate to diabetes and obesity. The areas investigated include the roles that changes in the blood-to-brain transport of leptin, ghrelin, and insulin play in obesity & anorexia to the disruption of the blood-brain barrier that occurs in diabetes.

Ernie Blevins, PhD
View Department Profile
The obesity epidemic and its associated complications have become major health concerns, highlighting the need to develop new and effective strategies to treat obesity
The research in my lab focuses on understanding the mechanisms that contribute to the ability of the hypothalamic neuropeptide, oxytocin, to elicit weight loss in diet-induced obese rodents and nonhuman primates.
Recent findings indicate that oxytocin may elicit weight loss, in part, by reducing food intake and by activating interscapular brown adipose tissue (IBAT) to increase energy expenditure.
We are currently focused on determining whether the effects of oxytocin to increase energy expenditure and elicit weight loss require activation of sympathetic outflow to IBAT and if reducing oxytocin signaling in a CNS site that controls BAT contributes to leptin resistance, obesity and the anti-obesity effects of chronic systemic oxytocin.
We will further investigate the translational question of whether chronic intranasal oxytocin elicits weight loss, activates BAT and improves glucose tolerance in a DIO nonhuman primate (rhesus monkey) model of metabolic syndrome.
These findings will direct future studies to address the extent to which intranasal oxytocin may reverse obesity in humans by stimulating BAT thermogenesis.

Mauricio Dorfman, PhD
View Profile
Assistant Professor of Medicine
Division of Metabolism, Endocrinology and Nutrition

Dianne Lattemann, PhD
View Department Profile
My lab has been interested in the effects of metabolism and metabolic hormones on aspects of brain function, including ingestive behaviors and responsivity to metabolic stressors such as hypoglycemia. Currently, we are interested in the effects of specific dietary fatty acids on brain function and behavior, including food reward behavior, and the cellular and nuclear mechanisms by which fatty acids may impact on CNS function (epigenetic and gene expression changes).

Gregory Morton, PhD
View Profile
Associate Professor of Medicine
Division of Metabolism, Endocrinology and Nutrition
Christian Roth, PhD
View Department Profile
In recent years, my research has been focused on childhood obesity, including, functional neuroimaging of brain regions involved in appetite control as well as translational studies regarding metabolic changes associated with childhood obesity and risk for type 2 diabetes development. I am interested in evaluating neurobiological and metabolic risk factors before and after weight loss due to lifestyle intervention in obese children. In my lab, we analyze different peptides involved in the regulation of food intake and energy homeostasis, and we also test different agents as potential anti-obesity drugs.

Jarrad Scarlett, MD, PhD
View Profile
Assistant Professor of Pediatrics
Division of Division of Gastroenterology & Hepatology

Michael Schwartz, MD
View Profile
Co-Director, UW Diabetes Institute
Professor of Medicine
Division of Metabolism, Endocrinology and Nutrition

Ellen Schur, MD, MS
View Profile
Director, Clinical Research Unit, UW Diabetes Institute
Associate Professor of Medicine
Division of General Internal Medicine

Joshua Thaler, MD, PhD
View Profile
Associate Professor of Medicine
Division of Metabolism, Endocrinology and Nutrition

Brent Wisse, MD
View Department Profile
Dr. Wisse’s research focuses on identifying key CNS signals whereby systemic inflammatory mediators cause anorexia and weight loss, including cachexia – the specific wasting of skeletal muscle.
Glucose Homeostasis and Diabetes Pathogenesis

Laura den Hartigh, PhD
View Profile
Associate Professor of Medicine
Division of Metabolism, Endocrinology and Nutrition

Jose Garcia, MD, PhD
View Department Profile
Dr. Garcia is a translational researcher working on the role of ghrelin and other anabolic therapies in regulating appetite and body composition in the setting of sarcopenic obesity and other wasting disorders.

George Ioannou, MD, MS, FAASLD
View Department Profile
Dr. Ioannou is the Director of Hepatology at the VA Puget Sound and Co-Director of the VA's Hepatic Innovation Team for Network 20. He is a Professor of Medicine at the University of Washington and Chair of the AASLD Practice Guidelines Committee. His research interests include the role of cholesterol in the pathogenesis of NASH, the use of prediction models in liver disease, and the epidemiology of hepatocellular carcinoma.
Brian Iritani, DVM, PhD
View Department Profile
The Iritani lab studies the normal functions of oncoproteins and other signaling molecules in the development and function of immune cells, and how when dysregulated, aberrant expression or activity can result in autoimmune diseases or cancer. The Iritani lab has more recently focused on molecules that control immunometabolism, as well as skeletal muscle, cardiac muscle, and whole-body metabolism.

Mario Kratz, PhD
View Department Profile
Dr. Kratz’s research is focused on the relationship between diet, obesity, and chronic diseases associated with obesity, including type 2 diabetes, cardiovascular disease, and cancer. His group conducts randomized controlled clinical feeding trials and other clinical and observational studies to improve our understanding of the relationship between diet, obesity, and chronic disease. One particular focus is on low-grade chronic adipose tissue inflammation and non-alcoholic fatty liver disease as crucial mechanistic links between diet composition, obesity, and disease.
Daniel Raftery, PhD
View Department Profile
Our group focuses on developing methods and applications in the field of metabolomics, which provides a broad view of both normal and altered metabolism in a ranges of diseases, including diabetes. Metabolomics helps us identify the effects of biological stresses such as diabetes on cellular metabolism, and to identify disease biomarkers as well as metabolic vulnerabilities to target for therapy. Our current focus is probing the role of altered mitochondrial metabolism in driving a number of disease related processes.

Katya Rubinow, MD
View Profile
Assistant Professor of Medicine
Division of Metabolism, Endocrinology and Nutrition
Hormones, Nutrition and Diabetes

Bradley Anawalt, MD
View Department Profile
Dr. Anawalt's primary research interests are focused on the effects of testosterone in men.
Judy Chen, MD, FACS, FASMBS
View Department Profile
Dr. Chen's clinical interests include advanced minimally invasive gastrointestinal surgery and laparoscopic metabolic weight management surgery.

Karen Foster-Schubert, MD
View Department Profile
My research interests regarding diabetes fall within the realm of understanding the role of bariatric/metabolic surgery to contribute to type 2 diabetes remission and amelioration. I am also interested in the epidemiology of bariatric/metabolic surgery within the Veteran population with type 2 diabetes, particularly with regards to policy impacts.

Nina Isoherranen, PhD
View Department Profile
Dr Isoherranen’s laboratory focuses on understanding how vitamin A homeostasis is altered in obesity and related comorbidities and how obesity and diabetes are related to alterations in vitamin A balance in humans. Her laboratory has ongoing research projects on physiologically-based pharmacokinetic modeling of how drug disposition changes in various disease states including diabetes and its comorbidities.

Saurabh Khandelwal M.D., FACS, FASMBS
View Department Profile
Dr. Khandelwal’s research interests involve collaboration with the departments of medicine and endocrinology looking at the effects of bariatric surgery on central nervous system changes, as well as the effects of bariatric surgery on micronutrient metabolism. In addition, his research interests lie in outcomes research and bariatric surgery.

Stephanie Page, MD, PhD
View Profile
Co-Director, UW Diabetes Institute
Professor of Medicine
Head, Division of Metabolism, Endocrinology and Nutrition